Diabetes (lat. Diabetes mellitus) is a chronic disease from the group of endocrine diseases whose most important feature is elevated blood glucose level (hyperglycemia) resulting from a disorder in hormone insulin secretion or action.
 According to the classification of the World Health Organization, diabetes is subdivided into type 1 diabetes and type 2 diabetes. Looking at the total number of patients suffering from this disease, with type 1 diabetes is affected only 5 to 10%, while diabetes type 2 affects 90 to 95% of these patients. In type 1 diabetes there is an autoimmune destruction of pancreatic beta cells (which produce hormone insulin) and this form of the disease usually occurs in childhood and adolescence. In the background of type 2 diabetes there is a disturbed secretion or function of insulin. The frequency of this type of diabetes increases with age, obesity and physical inactivity, and there is also a genetic predisposition as well.
According to the classification of the World Health Organization, diabetes is subdivided into type 1 diabetes and type 2 diabetes. Looking at the total number of patients suffering from this disease, with type 1 diabetes is affected only 5 to 10%, while diabetes type 2 affects 90 to 95% of these patients. In type 1 diabetes there is an autoimmune destruction of pancreatic beta cells (which produce hormone insulin) and this form of the disease usually occurs in childhood and adolescence. In the background of type 2 diabetes there is a disturbed secretion or function of insulin. The frequency of this type of diabetes increases with age, obesity and physical inactivity, and there is also a genetic predisposition as well.
Furthermore, diabetes may occur as a result of pregnancy, endocrinopathy (disease of an endocrine gland, the term is commonly used as a medical term for a hormone problem) and as a result of taking certain medications.
The hormone insulin is produced in the beta cells of the pancreas and is secreted in response to elevated blood sugar level. Insulin promotes the entry of sugar into cells and it’s storage in the liver in the form of glucagon. In addition, insulin can affect the metabolism of free fatty acids and amino acids. If there is not enough insulin, or it does not achieve its function, the cells of the body can not exploit blood sugar as an energy source, and for this purpose they break down triglycerides from fat tissue into fatty acids.
 Diabetes is a disease of modern age. Although diabetes can affect any age group, it’s incidence increases with age. Today, International Diabetes Federation estimates that worldwide more than 380 million people have diabetes, which is about 8.3% of humanity.
Diabetes is a disease of modern age. Although diabetes can affect any age group, it’s incidence increases with age. Today, International Diabetes Federation estimates that worldwide more than 380 million people have diabetes, which is about 8.3% of humanity.
The diagnosis of diabetes is set based on the measurement of glucose level (sugar) in the blood and the result of glucose tolerance test (OGTT). If the values of randomly measured blood glucose levels are 11.0 mmol/L or more, and a fasting blood glucose is 7.0 mmol/L or more, repeated in at least two independent measurements, that indicate impaired glucose tolerance in the body and it is necessary to make additional tests to establish the diagnosis.
The main clinical feature of diabetes is elevated blood sugar level!
The excess sugar in the blood is excreted through the kidneys and urine (glycosuria), which causes osmotic diuresis and frequent urination (polyuria), and this leads to dehydration and the abnormally great feeling of thirst (polydipsia) and the consequent loss of body weight.
Acute complications are hypoglycemia and hypoglycemic coma, diabetic ketoacidosis and diabetic ketoacidotic coma and diabetic hyperosmolar coma. However hypoglycemia is the most common acute complication in patients on insulin therapy. Symptoms of hypoglycemia occur when blood sugar levels are less than 2.5 mmol/L.
The chronic complications are divided into macrovascular and microvascular. Macrovascular complications include ischemic heart disease and cerebrovascular and peripheral vascular disease. Patients with diabetes often have a harder and more extensive atherosclerotic changes in the coronary arteries, and increased risk of heart attack. Microvascular complications such as retinopathy, nephropathy and neuropathy appear at a younger age and are more severe in patients with type 1 diabetes. Diabetes is the leading cause of visual impairment and blindness, which is 25 times more common in people with diabetes than in the general population.
- Package Contents: you will receive 12 awareness enamel lapel pins, each carefully picked with different colors symbolizing various meanings of support; Wearing this hope ribbon collar pin can increase people's awareness of multiple cancers and diseases; They are stored in an exquisite transparent box, well preserved, abundant in quantity, and can meet your daily needs and sharing requirements
- Material and Size: this prevention and awareness pins are crafted with professional techniques, made of zinc alloy material, ensuring quality and long term use; They are resistant to wear and fading, sturdy and durable; The size is approximately 1.18 x 1.18 inches/3 x 3 centimeters, suitable for most people to wear
- Colorful Design: this hope ribbon brooch badge pins are designed with 10 colors of red for oral cancer, white for lung cancer, pink for breast cancer, dark blue for colorectal cancer, green for liver cancer, yellow for childhood cancer, purple, light khaki wine red, and light purple ribbons surrounding the word "hope", expressing a clear message; The colors are vibrant and eye catching
- Secure Clutch Back: our hope ribbon brooch badge pins are equipped with a convenient clutch back, also known as a military clutch back; It includes an anti rotation spike to enhance safety and can securely fasten to clothing, bags, or hats; Simply press down the wings on the side of the backing gently
- Versatile Usage: these prevention and awareness pins are suitable gifts for fundraising events, business activities, charity events, holiday commemorations, and prevention campaigns; They can be given to friends, colleagues, and people you care about, expressing your support and warmth
- Green is the new White. Our Whitening Strips will effectively whiten your teeth without harming your oral health. Our Green Whitening Strips have natural stain remover and no sensitivity side effects. Use 30 minutes each day for 14 days to achieve a whiter, brighter smile.
- Non-Peroxide Whitening: Achieve a brighter smile without the use of hydrogen peroxide, which can cause sensitivity for some users. Our formula provides effective whitening while being gentle on your teeth and gums. It’s also SLS-free (Sodium Lauryl Sulfate), ensuring a milder, non-irritating experience, and contains no alcohol, making it more safe and non-drying for everyday use. Perfect for those who looking for a more natural whitening solution.
- Powered by a natural brightener from Bearberry, green antioxidants and Coconut Oil. All these ingredients are combined to bring you whiter teeth and a brighter smile.
- Laboratory Tested. All ingredients have been thoroughly tested by an accredited independent laboratory. That means that our products are certified and safe for your oral health.
- Good Taste and Enamel Safe. It’s strong enough to remove stains, yet not so strong to cause harsh bleaching effects or sensitivity. The teeth whitening strip is enamel-safe, providing you with a pleasant teeth whitening experience. Great coconut mint flavor because whitening can be tasty too
- What You'll Get: One (1) box of 36 Dry Mouth Lozenges with Xylitol, Soothing Mint Flavor
- Sugar-free Lozenges: ACT Dry Mouth Lozenges do not contain fluoride
- Benefits: Soothes dry mouth, moisturizes mouth tissue and freshens breath
- Convenient Relief: Take with you for dry mouth relief anytime, anywhere
- Soothe Dry Mouth: Alleviate the symptoms of dry mouth with ACT Xylitol-infused lozenges
 Dental treatment of patients with diabetes
Dental treatment of patients with diabetes
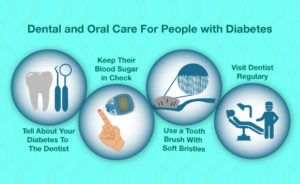
The dentist should from each patient who had first come to dental exam or since last visit has been more than 12 months, take a detailed medical history. A patient who is being treated for diabetes should inform the dentist in detail about the medications he uses, as well as the regularity of their taking. Each dental patient in which there are symptoms suspect of diabetes (such as polydipsia (excessive thirst), polyuria (frequent urination), polyphagia (excessive hunger), weight loss and weakness) should be referred to a physician for further examination, certainly before the start of extensive dental procedures. In addition, the dentist should bear in mind that a high risk of developing diabetes have persons whose parents are suffering from diabetes, women who have given birth to one or more children with an extremely large body weight, women who had a miscarriage, obese people and people older than 40 years with an unhealthy lifestyle, diet and with insufficient physical activity.
In patients with well-controlled insulin independent diabetes can all dental procedures without any special restrictions can be performed. The same goes for patients with well-controlled insulin-dependent diabetes.
 To be able to say that diabetes is well controlled, the concentration of glucose in the blood must be in the normal range, the patient must have normal blood pressure and may not have diabetic complications such as heart attack, cardiac arrhythmia, kidney problems and others. If the patient has one or more diabetic complications, dental procedures are planned and executed in accordance with his or her health status, which, if necessary, may include cooperation with the patient’s physician.
To be able to say that diabetes is well controlled, the concentration of glucose in the blood must be in the normal range, the patient must have normal blood pressure and may not have diabetic complications such as heart attack, cardiac arrhythmia, kidney problems and others. If the patient has one or more diabetic complications, dental procedures are planned and executed in accordance with his or her health status, which, if necessary, may include cooperation with the patient’s physician.
For patients with diabetes it is better to schedule dental appointments in the morning. Before visiting, the patient should take his usual dose of insulin on a regular schedule and should have breakfast.
If during the implementation of dental treatment the patient notices any unusual changes, symptoms or nausea, he should immediately inform the dentist. In this case, the procedure is temporarily interrupted or postponed, and the patient is offered to drink a sweetened beverage. When planning extensive oral surgery procedure, it is advisable to consult the patient’s physician about the diet in the postoperative period.
 In some patients with type 1 diabetes who are receiving high doses of insulin, periods of extreme hyperglycemia or hypoglycemia may occur, even if the disease is under complete control. In such patients, as well as in those who in addition to diabetes have chronic oral infection, during oral surgery it is necessary to apply an appropriate antibiotic prophylaxis.
In some patients with type 1 diabetes who are receiving high doses of insulin, periods of extreme hyperglycemia or hypoglycemia may occur, even if the disease is under complete control. In such patients, as well as in those who in addition to diabetes have chronic oral infection, during oral surgery it is necessary to apply an appropriate antibiotic prophylaxis.
In most patients with diabetes local anesthetics can be used without particular limitations. However, it should be kept in mind that adrenaline from local anesthetic has pharmacological activity against the action of insulin, so blood sugar level may increase if the anesthetic with adrenaline is used. Patients who in addition to diabetes have high blood pressure, cardiac arrhythmia or recently had a heart attack, a local anesthetic with adrenaline should be used with caution as their blood pressure may not be further increased.
Oral health of individuals with diabetes
Manifestations of diabetes in the oral cavity can be multiple. One of the first characteristics is the feeling of dryness in the mouth or xerostomia. Because of diabetic angiopathy and neuropathy, there is a disturbance in the work of the salivary glands, resulting in reduced secretion of saliva.
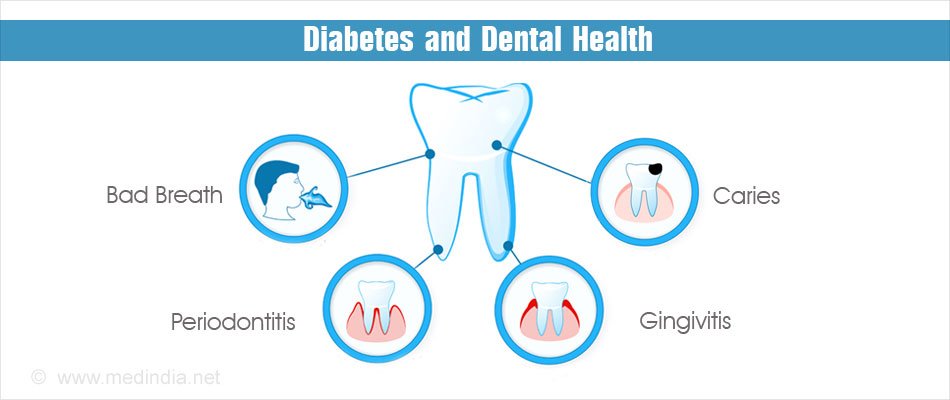 Reduced amount of saliva causes a number of other, mostly non-specific disorders in the oral cavity, such as burning sensations of mucous membranes (burning mouth syndrome), changed sense of taste (dysgeusia or ageusia) and disturbances in chewing and swallowing because there is lack of saliva that lubricates the mucous membranes. In addition, by reducing the amount of saliva, mechanical self-cleaning of teeth with spray of saliva is also missing. Due to this, there is accelerated plaque accumulation on the teeth and consequently development of dental caries. As there are numerous factors in saliva that normally protect the mouth against bacterial, viral and fungal infections, by reducing the amount of saliva proportionately decreases its protective effect and increasing susceptibility to infections. Furthermore, in saliva of patients with diabetes levels of glucose and calcium are elevated, which leads to acid-base imbalance and acid reaction, and this further increases the risk of developing infections of the oral mucosa.
Reduced amount of saliva causes a number of other, mostly non-specific disorders in the oral cavity, such as burning sensations of mucous membranes (burning mouth syndrome), changed sense of taste (dysgeusia or ageusia) and disturbances in chewing and swallowing because there is lack of saliva that lubricates the mucous membranes. In addition, by reducing the amount of saliva, mechanical self-cleaning of teeth with spray of saliva is also missing. Due to this, there is accelerated plaque accumulation on the teeth and consequently development of dental caries. As there are numerous factors in saliva that normally protect the mouth against bacterial, viral and fungal infections, by reducing the amount of saliva proportionately decreases its protective effect and increasing susceptibility to infections. Furthermore, in saliva of patients with diabetes levels of glucose and calcium are elevated, which leads to acid-base imbalance and acid reaction, and this further increases the risk of developing infections of the oral mucosa.
Oral candidiasis (Candida albicans) is a common finding in diabetics. Signs of this infection are evident on the tongue and at the corners of mouth, but in people with dentures they can also be found on hard palate and on oral tissues under the denture base. Due to reduced immune response infection often recur. In addition, during and after antifungal therapy against oral candidiasis, patients with diabetes may develop bacterial infections resistant to therapy.
Increased accumulation of plaque and tartar due to decreased saliva secretion and microvascular changes that accompany diabetes gradually lead to major changes in the periodontium (oral structures that surround teeth) – periodontitis. Initially there is hyperemia (red gums) with gingivitis of the gums, which eventually progress towards periodontitis with periodontal pockets and alveolar bone destruction. Absence of periodontal treatment and adequate therapy causes the teeth to become movable and easily fall out.
 The sweet, acetone breath (foetor ex ore – bad breath), which appears as a result of ketoacidosis process in the body, is one of the specific features of diabetes and is considered as characteristic sign that certainly points to diabetes.
The sweet, acetone breath (foetor ex ore – bad breath), which appears as a result of ketoacidosis process in the body, is one of the specific features of diabetes and is considered as characteristic sign that certainly points to diabetes.
Changes in the oral cavity that appear as a result of diabetic disease are treated by general dentist and very often in cooperation with the specialist in oral medicine. It is especially important to remove all the local irritation in the mouth because the mucus membranes are easily vulnerable, prone to infection and difficult to heal. Regularly and properly conducted oral hygiene is the foundation to preserve good oral health in these patients. Depending on the type and intensity of the manifestations of diabetes in the oral cavity, the appropriate therapeutic procedures should be taken. Inflammatory changes are treated, depending on the cause, with antimycotic (antifungal drug) in suspension or gel, or with antibiotics in the form of ointments or creams. Rinsing with oral antiseptics and unsweetened tea is recommended in order to act anti-inflammatory and to provide hydration of oral mucosa. If necessary, preparations of artificial saliva can be used in order to compensate inadequate secretion of saliva.
Conclusion
Diabetes is a disease of modern man with a growing increase in the number of patients. The disease is accompanied by numerous acute and chronic complications that may very badly affect the quality of daily life of the individual suffering from diabetes. Manifestations of diabetes in the oral cavity are multiple, although mostly nonspecific. The sweet acetone smell from the mouth is considered as characteristic sign that refers to diabetes. With cooperation between the dentist specialist in oral medicine and medical doctor diabetologist, it is possible to preserve and enhance patient’s oral health, which significantly improves the quality of everyday life.