Table of Contents
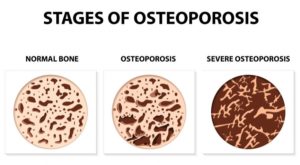
Osteoporosis is the most common metabolic bone disease where a gradual and initially imperceptible loss of bone mass occurs. In this disease, the activity of osteoclasts (cells that biodegrade bone) and osteoblasts (cells that build bone) is out of balance. Namely, the osteoclasts degrade significantly more bone than the osteoblasts are able to restore and compensate as is normally the case in healthy people. It is believed that between the twentieth to thirtieth years of life amount of bone mass in human body stabilizes and settles, and without major changes remains the same to fortieth. After forty years of age, bone mass begins to decrease for about 1 percent a year.
Osteoporosis and teeth problems affects millions of people, including more than one third of women older than 65 years. It is estimated that in the United States it affects more than 10 million of people, and causes more than 2 million fractures annually. In another 34 million Americans, the reduced bone density and increased risk of osteoporosis dental implications are identified. Although there is no uniform system of registering patients with osteoporosis, or people with fractures caused by the same condition, one of the biggest USA epidemiological studies of osteoporosis discovered that, based on ultrasound densitometry, it is found in 38.6 percent of respondents. It is believed that the prevalence of osteoporosis in USA is from 10 to 15 percent, and that corresponds to the figure recorded in other European and Asian population. As you can see osteoporosis and teeth breaking are very much connected.
For women in menopause, osteoporosis is usually caused by a decrease in estrogen levels, while after seventy years of age senile osteoporosis appears as a result of lower metabolism of calcium.
There are many states and cases which may cause this medical condition: early entry into menopause, surgical removal of ovaries before menopause, unbalanced menstrual cycle, anorexia, alcoholism, smoking, genetic predisposition, lack of physical activity, certain medications and excessive caffeine intake. Osteoporosis and teeth problems can also affect men , which is usually accompanied by a loss of testosterone, and as the most important factor that contributes to its development is mentioned alcoholism.
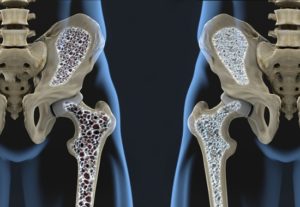 The gradual weakening of the bones, which is usually not accompanied by other symptoms, comes to light the moment when bone fracture occurs in normal life activities. Fractures most often occur on vertebrae and pelvic bones and forearm which significantly affects quality of life, and fractures of the spine or pelvis can cause complications or death.
The gradual weakening of the bones, which is usually not accompanied by other symptoms, comes to light the moment when bone fracture occurs in normal life activities. Fractures most often occur on vertebrae and pelvic bones and forearm which significantly affects quality of life, and fractures of the spine or pelvis can cause complications or death.
Osteoporosis can be most reliably diagnosed by measuring bone mineral density which is called bone densitometry (ultrasound or DXA – Dual-energy X-ray absorptiometry). Osteoporosis can be prevented and treated, and therefore, patients should regularly consult a doctor and follow the doctor’s instructions. To raise the level of global awareness about the prevention, diagnosis and treatment of osteoporosis and other metabolic bone diseases, since 1996, on the initiative of the International Osteoporosis Foundation, every year on October 20 the World Day of osteoporosis is marked.
Symptoms of osteoporosis usually remain unnoticed for a long time, until a larger bone fracture occurs. The dentist, during a regular dental exam, can detect early changes in oral cavity that may indicate the presence of osteoporosis. Thanks to early detection of osteoporosis, it is possible to successfully treat and avoid many complications which the disease can cause. Does osteoporosis affect teeth? Read the next chapter to find out.
Can osteoporosis affect teeth?
Early signs in the mouth that may indicate the presence of osteoporosis are: loose teeth, periodontal disease, dentures which are not well-fitting due to rapid degradation of the jaw bone and difficulties with eating and speaking.
If the dentist discovers any sign which could be susceptible to osteoporosis, he will need to make dental X-rays to determine the density of the jaw bones and also possibly determine the cause of dental disorders. In addition, periodically taking X-rays of the teeth and jaws for the needs of dental treatment allows the dentist to monitor changes in jaw bone density over a period of time.
 In the advanced stage this disease can lead to severe periodontal disease, tooth loss and accelerate the disappearance of alveolar bone of the jaw. Osteoporosis and tooth loss are common. Due to the gradual disappearance of the alveolar bone, making and wearing prosthetic appliances (dentures) are becoming more difficult, there are disturbances in the consumption of food and beverages and in speech.
In the advanced stage this disease can lead to severe periodontal disease, tooth loss and accelerate the disappearance of alveolar bone of the jaw. Osteoporosis and tooth loss are common. Due to the gradual disappearance of the alveolar bone, making and wearing prosthetic appliances (dentures) are becoming more difficult, there are disturbances in the consumption of food and beverages and in speech.
Bisphosphonates and osteonecrosis of the jaw
Many people with low bone density and/or osteoporosis receive drugs from the group of bisphosphonates (alendronate, ibandronate, risedronate, etidronate, raloxifene, etc.) that successfully increase bone density and prevent the occurrence of fractures.
In recent years, in technical and scientific literature we can more often find reports on cases of osteonecrosis of the jaw in patients who were treated with bisphosphonates.
The bisphosphonate-related osteonecrosis of the jaw (bisphosphonate-associated osteonecrosis of the jaw), though it is still relatively rare but at the same time very serious condition, can cause great damage to the jaw bone. To diagnose osteonecrosis of the jaw caused by bisphosphonates, the patient must be treated with bisphosphonates, open bone lesions of jaw bones should be present for more than eight weeks and in the medical history patient should not have any record of having been subjected to radiation of the head and neck.
A drug that will soon replace bisphosphonates in the treatment of osteoporosis is already increasingly mentioned – denosumab (receptor activator of nuclear factor kappa-B inhibitor ligand – RANKL inhibitor). Advantages of denosumab, compared with bisphosphonates, are considerably fewer side effects. However, the risk of osteonecrosis of the jaw still persists and with this new drug, so that additional testing is required.
The patient is required to inform his dentist about all medications he takes, including those relating to the treatment of osteoporosis.
Considering the increasing number of drugs and medical preparations on the market, it is recommended that patients write a list of medications they take and that the list becomes a part of the patient’s dental records. People with osteoporosis and tooth decay should specifically warn their dentist if they are taking bisphosphonates or other antiresorptive drugs. It is not advisable that, due to dental treatment, patients decide on their own to discontinue osteoporosis treatment, because the risk of developing osteonecrosis of the jaw is considerably less than the possible risks and complications that untreated osteoporosis may lead.
Dental treatment
Some dental procedures in people with osteoporosis are associated with an elevated level of risk of developing certain complications. These complications are not so much related to the nature of the disease, but more with the drugs used in the treatment, primarily bisphosphonates as the most common remedy for osteoporosis.
Preventive dental procedures, conservative treatments, endodontic treatments, non-invasive periodontal procedures and making the prosthetic replacement (dentures and bridges) in people with osteoporosis usually can be carried out without any special restrictions.
Orthodontic treatment is not contraindicated, but still it is preferable that, in planning orthodontic treatment in patients with osteoporosis, the dentist and the doctor who treated the patient with osteoporosis consult and identify potential risks to which orthodontic treatment can lead. In this way, it is possible to prevent and/or reduce any adverse effect of orthodontic treatment.
Invasive dental procedures such as oral surgical and periodontal-surgical procedures should be carefully planned considering the risk of osteonecrosis of the jaw caused by bisphosphonates.
Tooth extraction is considered the main cause of the occurrence of osteonecrosis of the jaw caused by bisphosphonates. According to some studies, 60 percent of cases of osteonecrosis of the jaw caused by bisphosphonates appears after tooth extraction, while the remaining 40 percent occurs spontaneously and unrelated to tooth extraction and are associated with wearing dentures that are considered as a potential source of local trauma.
Osteoporosis and dental implants
Implant placement procedure in the jaw bone is also very risky with these patients. The risk of osteonecrosis of the jaw is not only an act of implant placement, but also an implant itself is a permanent local risk factor.
Preventive oral hygiene measures
People with osteoporosis and a predisposition to its development should take food rich in calcium and vitamin D (milk and dairy products, broccoli), avoid fizzy drinks as phosphoric acid can prevent the absorption of calcium, regularly engage in any physical activity, less smoke and less consume alcohol, and of course abide by the advice and instructions of doctor.
All general oral hygiene preventive measures (regular tooth brushing, flossing and using of interdental brush) healthy diet and regular dental visits are also valid for people with osteoporosis teeth problems. However, these patients should intensify care of their oral health, because if a need for invasive dental procedure appears, such as tooth extraction, there is an increased risk of complications of the primary disease and the occurrence of osteonecrosis of the jaw.
Conclusion
Osteoporosis is a common disease of modern age, and primarily affects women. Given the fact that the early signs of osteoporosis can be spotted in the oral cavity, the dentist is able to identify patients with osteopenia and osteoporosis, alert them to the possibility of developing the disease and direct to further treatment. It would be good for patients to visit their dentist before starting bisphosphonate therapy or shortly after the start of treatment, in order to verify the state of their osteoporosis and oral health and reduce the chance of developing osteonecrosis of the jaw.